

We review here what has been learned to date from the development and implementation of SCID NBS.
9- 14 Some programs point to particular local issues that make TREC screening even more important, such as founder mutations or high rates of consanguineous marriage. 8 These and other publications have also addressed a range of non-SCID conditions that can be found in infants who have an abnormal SCID NBS result, but do not have SCID.Īs of this writing, multiple nations around the world have instituted population-wide NBS for SCID, including New Zealand, Israel, Sweden and Germany, while others offer SCID screening in limited areas or have published pre-implementation analyses and pilot studies, all with enthusiastic support. 7 An additional recent publication of results from screening over 3.2 million infants in California confirmed a similar incidence of 1/65,000 births, with 96% survival.

Further, the survival of infants who received HCT, gene therapy (GT) or enzyme replacement therapy, for adenosine deaminase (ADA) deficient SCID, was 92%, in contrast with prior reports and current data of around 70% in a large European study of SCID HCT without NBS. 6 They found that the incidence of SCID was 1/58,000, nearly double what had been estimated from previous studies. In 2014, the newborn screening programs from 10 states and the Navajo Nation, which were early to adopt SCID NBS, reported their pooled experience.

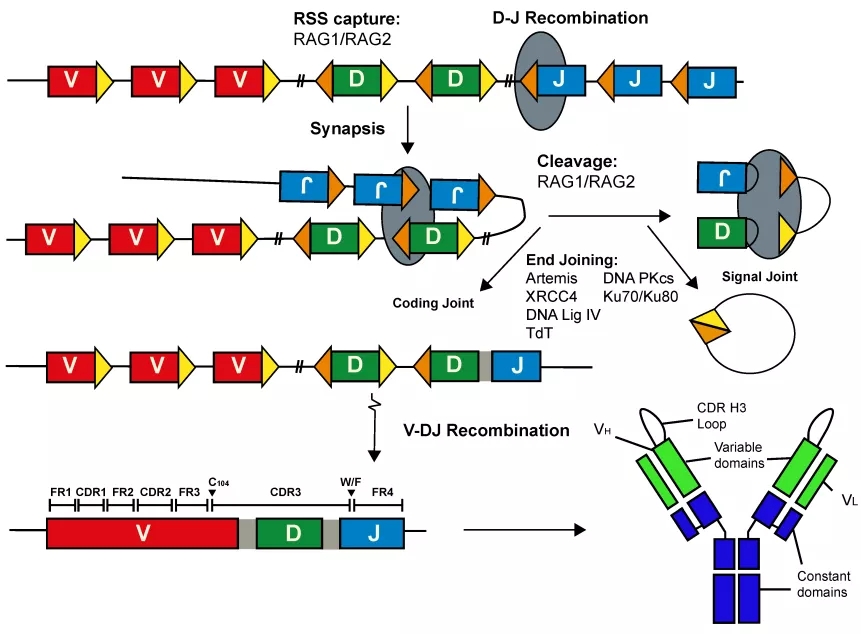
These non-specific indications led to delays in recognition of the underlying cause and subsequent delays in treatment, with HCT often performed only after the patient had acquired devastating infections that compromised outcomes. 4 Infants with SCID appear healthy as newborns and, prior to SCID NBS, were diagnosed only after frequent medical encounters for recurrent and persistent infections, infections with opportunistic organisms, and/or failure to thrive. 3 However, a large majority of SCID cases are sporadic, with no recognized family history to prompt early diagnosis. 2 SCID is caused by mutations in any of over 20 genes governing the differentiation and proliferation of mature lymphocyte lineages derived from hematopoietic stem cells (HSC) in the bone marrow. The case for SCID NBS arose from data showing improved survival of infants recognized by a positive family history and treated with life-saving hematopoietic cell transplantation (HCT) therapy within the first 3.5 months of life, compared to infants diagnosed and treated later, after suffering increasingly severe and debilitating infections. With NBS in place, the overwhelming majority of infants with SCID are identified by screening instead of by the classical presentation with infectious complications. Indeed, by the end of 2018, NBS for SCID had been adopted by public health programs in all 50 states, the Navajo Nation and Puerto Rico. 1 This marked a watershed in the diagnosis and treatment of SCID in the United States. In 2010, severe combined immunodeficiency (SCID) was added to the national list of conditions for which newborn screening (NBS) should be conducted, called the Recommended Uniform Screening Panel (RUSP), based on findings of the Advisory Committee for Heritable Disorders of Newborns and Children to the Department of Health and Human Services.


 0 kommentar(er)
0 kommentar(er)
